The Ash Center for Democratic Governance and Innovation sat down with Katharine Robb, a postdoctoral research fellow at the center’s Bloomberg Harvard City Leadership Initiative where she has been conducting research on housing and health in Chelsea, Mass. This densely populated city adjacent to Boston has seen some of the worst COVID-19 infection rates in the state. Robb completed her doctorate in public health degree at the Harvard T.H. Chan School of Public Health in 2019.
While pursuing her doctorate, Robb worked as an Innovation Field Lab fellow in Chelsea, ultimately focusing her dissertation on her work with the field lab, where she developed and implemented a novel social-service referral program within the city’s Inspectional Services Department. The program leverages the unique role of housing inspectors to link at-risk residents with services to prevent problem properties and social and health crises.
Q&A
Katharine Robb
Ash Center: Were you at all surprised that Chelsea has become one of the centers of the COVID-19 outbreak in Massachusetts?
Robb: No, it’s not a surprise. We know that diseases of many kinds disproportionately impact poor communities, people of color, and people living in overcrowded conditions. Chelsea has all three of these. Having spent a great deal of time in Chelsea, I know first-hand the strength and vibrancy of its community and culture. But, not only does Chelsea have a population with a lot of risk factors for infection, but because of the density and housing conditions, there are also limitations on people’s ability to reduce their risk from infection.
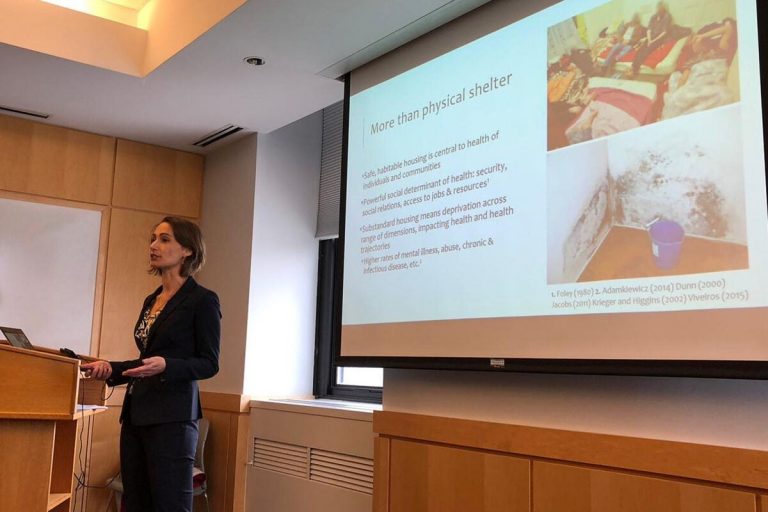
Ash Center: How do housing conditions impact health outcomes in urban environments?
Robb: Housing is so much more than physical shelter. It impacts every aspect of our lives, including our health in a really powerful way. It also impacts our security, our personal relationships, our privacy, and access to community resources. Housing related risks can stem from physical aspects of the home environment such as insect infestations that cause asthma attacks, or from financial aspects that result in poor property maintenance and create unsafe conditions in the home. Overcrowded conditions may strain interpersonal relationships or contribute to abuse or mental health problems.
Ash Center: Specifically, how have housing conditions in Chelsea possibly exacerbated the spread of the virus?
Robb: Even before the pandemic, homes were not a safe place for many residents in the city. Chelsea is the most densely populated city in Massachusetts, and one of the densest in the country. Many of the homes in Chelsea are two bedrooms or fewer, and contrary to national trends, family size in Chelsea is actually growing — so the housing stock really doesn’t match the needs of the current population in the city.
Chelsea is also emblematic of the affordable housing crisis that’s facing many cities where skyrocketing rents and stagnant wages increase the proportion of residents who lack adequate housing. Residents often cope with this by doubling or tripling up with other families and living in some really inhumane conditions such as unfinished basements or closets or porches, often lacking adequate water, sanitation, ventilation or heat. Many are forced to share bathrooms or kitchens with other families or residents, making social distancing and proper sanitary practices difficult if not impossible in some situations. Finally, we’ve seen that many Chelsea residents living in overcrowded or substandard conditions are more likely to experience underlying health conditions due to poverty, reduced access to healthcare and food, and psychological stress — which put them at greater risk of infection
Ash Center: How have past pandemics historically shaped housing policy in cities, and is there a possibility that the crisis we’re in now may spark similar changes in the future?
Robb: I think this pandemic highlights how in some communities across the US, families still face many health and social challenges — think poor ventilation, overcrowding, inadequate access to sanitation — that were faced at the end of the 19th century — and are still associated today with higher rates of death and disease. History shows us that epidemics can be a real turning point in the ways that cities address health. One hundred fifty years ago it was epidemics such as cholera or tuberculosis that generated the political will to care about improving conditions among the urban poor. This was because more enfranchised or wealthier classes were also impacted, and this gave rise to publicly financed improvements in drinking water supplies, in sanitation, as well as building and housing codes to improve sanitary and health conditions.
As the 20th century progressed the health conditions changed and we saw dramatic reductions in mortality and morbidity in cities. Over the last 100 years, the wealthy were better able to isolate themselves from unsafe or unsanitary conditions in poor areas of cities. As a consequence, budgets for public health departments shrank, and there was less political will to continue to care about the health conditions among the poor. But pandemics like this really expose so many underlying vulnerabilities and shine a light on the unacceptable disparities within our communities. It’s my hope that the pandemic can really be a turning point once again, and a call for action for greater investment in improving conditions so that members of our community are no longer living without safe and sanitary shelter.
This interview has been edited for length and clarity.